Effects of temporal changes in resting heart rate on future diabetes-related outcomes
Background and aims: Most studies have analyzed the relationship between resting heart rate (RHR) measured at only one time point and future clinical events.
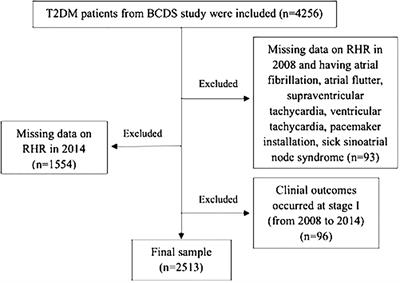
The current study aims to investigate the impact of long-term RHR changes on future clinical outcomes in a decade-long cohort with type 2 diabetes mellitus (T2DM). Methods: The two-staged follow-up involved 2,513 T2DM participants.
The first stage (2008-2014) intended to identify levels and trends in RHR changes, while the second stage (2014-2018) attempted to collect new occurrence records of clinical results. Cox proportional hazards models were applied to predict hazard ratios (HRs), along with 95% confidence interval (CI) for the correlation between RHR changes and future events. Results: There is no significant correlation between baseline RHR levels and long-term clinical events. According to the range of RHR change, compared with the stable RHR group, the adjusted HRs for cardiovascular events and all-cause death in the large increase group were 3.40 (95% CI: 1.33-8.71, p=0.010) and 3.22 (95% CI: 1.07-9.64, p=0.037), respectively. While the adjusted HRs for all-cause death and major adverse cardiac and cerebrovascular events (MACCE) in the moderate decrease group were 0.55 (95% CI: 0.31-0.96, p=0.037) and 0.51 (95% CI: 0.26-0.98, p=0.046). According to the trend of RHR, compared with the normal-normal group, the adjusted HRs for composite endpoint events and cerebrovascular events in the normal-high group were 1.64 (95% CI: 1.00-2.68, p=0.047) and 2.82 (95% CI: 1.03-7.76, p=0.043), respectively. Conclusion: Changes in RHR had predictive value for long-term clinical events in diabetic populations. Individuals with significantly elevated RHR over a particular period of time showed an increased risk of adverse events.
Read the full article at the original website
References:
