Kenya: Pandemic Health Workers Lack Protection
(Nairobi) – The Kenyan government has failed to fulfill its pledge to support health workers fighting Covid-19, exposing them to avoidable risks of trauma, infection, and even death, Human Rights Watch said today.
The government’s haphazard, uncoordinated response has affected the welfare of thousands of health workers, and hindered Kenya’s ability to provide timely and quality health care during the pandemic. Despite significant resources being dedicated to the Covid-19 response in Kenya, the government failed to provide health workers with adequate protective equipment, testing, or other safety measures to ensure that they could safely and effectively respond to the Covid-19 pandemic. President Uhuru Kenyatta ordered an investigation in August 2020 into the misuse of funds meant for the Covid-19 response.
The investigation found that Kenya had lost KSH7.8 billion (US$70.4 million) meant for Covid-19 response through corrupt tendering, but over one year later, no meaningful changes have resulted from the investigation. “Kenya’s negligence regarding the safety and needs of health workers in the middle of a pandemic is completely unacceptable,” said Otsieno Namwaya, East Africa director at Human Rights Watch. “Kenyan authorities should take urgent steps to ensure health workers on the front lines of the fight against Covid-19 are able to work in an environment that would not put them at unnecessarily heightened risk.” Kenya has 58,000 registered nurses, 12,000 registered doctors, and 14,000 clinical officers. Around 18,000 nurses are under government employment and thus went on strike during the Covid-19 crisis period, while 7,200 doctors are working in government facilities nationwide. Between March and July 2021, Human Rights Watch interviewed 28 government health workers and officials, including 14 nurses, 7 doctors, 3 clinical officers, 3 laboratory technicians, and a Health Ministry administrator. Six of the 14 nurses were union officials and four were officials of two different professional associations of nurses: National Nurses Association of Kenya (NNAK) and Kenya Progressive Nurses Association. Two of the seven doctors were union officials, and one was an official of the Kenya Medical Association (KMA), the country’s professional association of doctors. All union officials are active health workers. We also reviewed government documents, reports, records, and newspaper articles. Health workers said that at first, they did not have any personal protective equipment (PPE) – masks, gloves, or overalls/gowns. When they finally received equipment, there was either not enough or it was of poor quality.
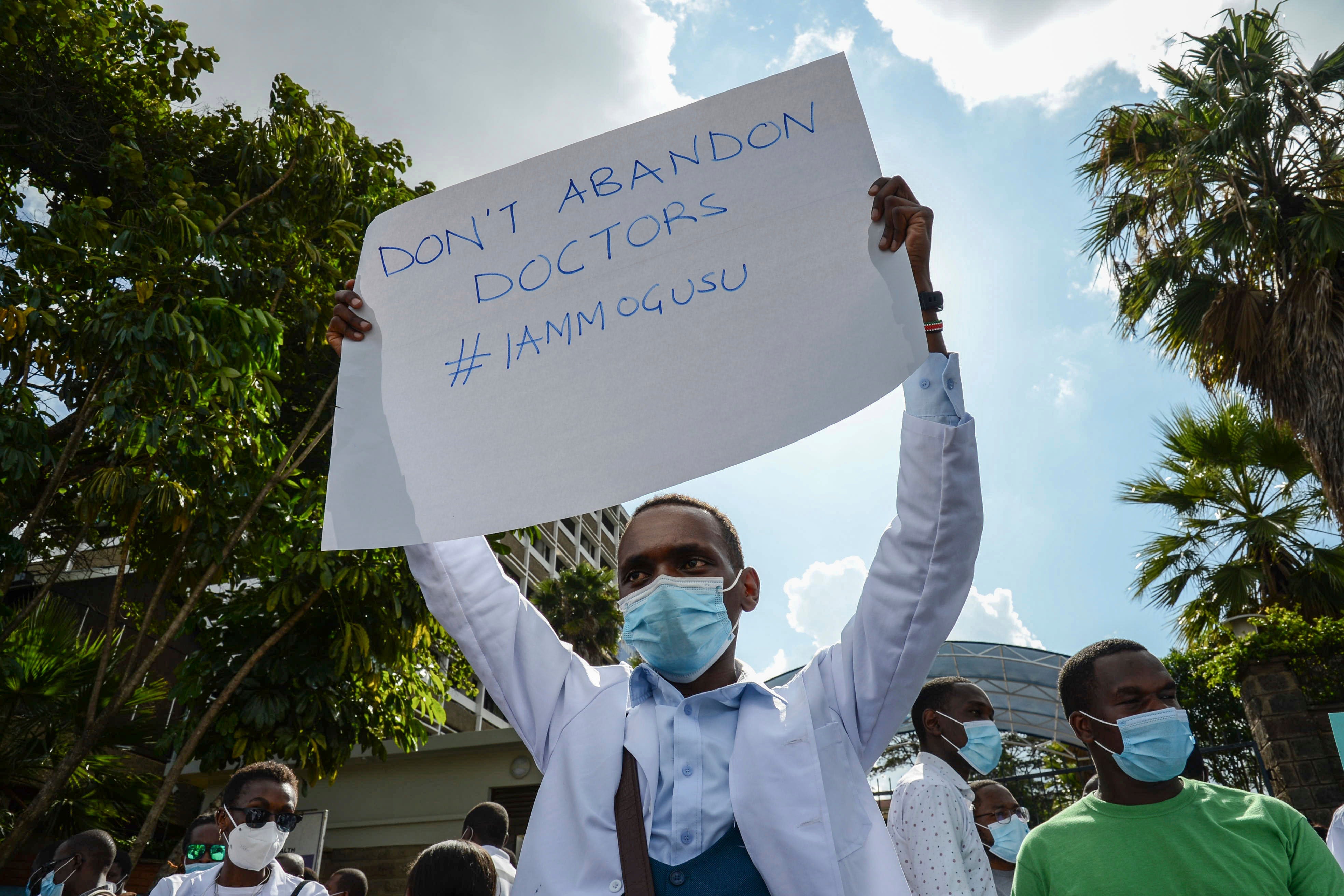
They said they did not receive training before being assigned to wards treating Covid-19 patients, greatly undermining their ability to respond in the early days of the pandemic. Fearing for their lives, some health workers said that they would sometimes panic and run away when they encountered people in the hospital with Covid-19-related symptoms. The lack of support led health workers nationwide to go on strike, with the nurses in at least five of the 47 counties starting the strike in June 2020 followed by doctors and clinical officers in August 2020.
The strike spread across Kenya quickly as health workers accused government of failing to address their grievances. Government addressed only some of the concerns, including provision of PPE to all health workers deployed to Covid-19 wards. Doctors responded by calling off the strike in December 2020, followed by nurses and clinical officers at the end of February 2021. Human Rights Watch research indicates that Kenyan authorities did not deliver on its promise to provide risk allowances; ensure that health workers hospitalized with Covid-19 had access to quality and affordable care; and that funeral expenses for the health workers who die from the disease would be covered. The doctors and nurses interviewed expressed disappointment that the authorities did not recruit enough staff, despite an available pool of trained but unemployed health workers to manage the expanded testing facilities. Nor, they said, did the authorities buy enough kits and reagents to ensure regular testing of everyone, including patients, staff at hospitals, and other members of the public. One doctor said that the limited availability of PPE made it difficult to observe basic safety protocols, such as regular replacement of PPE or having enough for all times on duty. All health workers interviewed said they felt overworked, stressed, and unsupported by the authorities, particularly because the authorities only recruited fewer than 1,000 nurses nationwide on one-year contracts, and underpaid them, and no new doctors to respond to the Covid-19 crisis. “We were being paid 10,000 Kenyan shillings [$100] per month, which we did not get for six months,” said one such newly contracted nurse. “The authorities gave us no risk allowances, no insurance, no health cover, no PPEs, and then we were placed at the emergency area where we were the most exposed.” An entry-level nurse at government hospitals earns about KSH51,600 ($516) per month and other allowances that could amount to almost the same amount. Three union officials said that several health workers attempted suicide due to the stressful work environment, but they did not provide details and Human Rights Watch could not independently confirm this. On July 19, Human Rights Watch wrote to Health Minister Mutahi Kagwe with a list of questions based on the findings and the issues raised by the health workers interviewed.
The ministry’s legal officer said, via phone, that the ministry could not comment because the issue of health supplies is still under investigation, referring to the investigation the president ordered. The Kenyan government should take urgent steps to ensure that those implicated in corrupt enrichment from Covid-19 funds are held accountable, Human Rights Watch said.
The authorities should also identify and address the systemic weaknesses that have facilitated corruption in the health sector and undermined the delivery of health services during the pandemic and beyond. Kenyan authorities have a responsibility to address these concerns both in the short, medium, and long terms, by urgently supplying materials health workers require to adequately respond to the ongoing Covid-19 crisis.
They should strengthen the health infrastructure and ensure accountability for malpractice, including corruption, that has negatively affected both supplies and access to adequate health care.
The authorities should consider allocating additional resources to the health sector to improve the overall quality of services. Under international and African law, Kenya has an obligation to minimize the risk of occupational diseases, including by ensuring that workers have health information, adequate PPE, and appropriate training in infection control.
The Kenyan government should, as a matter of urgency, allocate the necessary funds and resources to ensure that healthcare facilities have adequate equipment, supplies, and staff to ensure the highest possible quality care. “The government of Kenya owes doctors, nurses, and other health professionals, but also its global partners, corrective actions regarding its poor treatment of health workers,” Namwaya said. “The pandemic is still here, and the grave concerns of doctors and nurses should not be ignored.” For detailed findings and accounts by healthcare workers, please see below. Failure to Protect Health Workers Although Kenya pledged to assist health workers during the pandemic, the authorities did not carry out measures designed to create a safe work environment. Despite significant support from various donors, including the International Monetary Fund (IMF) and the World Bank, Kenyan authorities did not allocate enough funds to provide for adequate PPE, testing kits, and other safety measures to protect health workers against Covid-19 infections, causing them additional risk, mental trauma, and suffering. Medical supplies for public hospitals are procured centrally by the Kenya Medical Supplies Agency (KEMSA) and distributed to the hospitals. This severely reduced the availability of quality health care for Kenyans. On December 11, 2020, the Secretary General of the Kenya National Union of Nurses, Seth Panyako, indicated that its 23,000 members would only resume work after their demands were met, including providing PPE and the paying wages and allowances several months in arrears.
Their strike ended at the end of February 2021. When the health workers went back to work, it was out of necessity, although the authorities failed to address their grievances.
The health workers interviewed said that the government’s failure to ensure a safe, healthy work environment had potentially caused the deaths of more than 60 nurses and 35 doctors from Covid-19 by the end of 2020. President Kenyatta’s investigation into the misuse of funds meant for the country’s Covid-19 response unearthed that officials at the Kenya Medical Supplies Agency (KEMSA) had misappropriated at least 7.8 billion Kenyan shillings ($70.4 million) allocated for the Covid-19 response. Although the investigation recommended the prosecution of 15 government officials and businesspeople, causing KEMSA to reportedly suspend some of its board members and staff, the authorities have yet to charge anyone for the crimes. Inadequate PPE Human Rights Watch found that Kenyan authorities did not provide PPE to all health workers in time to prevent the spread of Covid-19 infections among them. Doctors, nurses, and laboratory experts said that by the time the government finally made supplies available, around June in many parts of the country, and July in others, only nurses and doctors in isolation wards received the equipment, mainly gowns, gloves and masks, which was of extremely poor quality. “Healthcare workers were given one overall and one mask to use for the whole day,” said one doctor, referring to the time the strike began in June 2020. “Whereas one gown should be used per incident, while masks are supposed to be changed regularly.” One doctor said that the PPE was of such low-grade materials, with large holes or openings, that it increased the probability of being infected. “It is more dangerous to use poor quality PPEs than not using them at all,” he said, “as the poor quality gear gives health workers the false sense of protection, which they don’t have.” The authorities also failed to ensure that all on-duty health workers had any form of PPE. An official of the professional body of nurses, National Nurses Association of Kenya (NNAK), expressed concern that the authorities were restricting the PPE to isolation wards: Everyone working at the hospital during the Covid-19 period should have PPE. It is difficult to know who in the general wards is safe and who is not. We are now at a higher risk of infection. We have colleagues who have been infected for unknowingly handling a Covid-19 patient. Health workers said that, while the authorities told health workers exposed to Covid-19 to self-isolate after working an extended period in the Covid-19 wards and before being in contact with their families, they failed to provide, monitor, or enforce the self-isolation protocol. Consequently, the families of health workers were exposed to a higher risk of infection.
The authorities created a network of health workers and community volunteers to visit those in self-isolation to ensure they adhered to the protocol, but these home visits never happened, those interviewed said. Health Workers Overworked, Untrained The health workers interviewed described being understaffed, under-equipped, and poorly trained. One senior nurse said that the government arbitrarily moved nurses to isolation wards without any orientation: With Corona, each of the 47 counties in Kenya now has ICU [intensive care unit] beds. But they are just moving nurses from the general wards to the ICU wards without any specialized training on the kind of care that is needed at the ICU/HDU [high-dependency unit] wards. On March 25, 2020, as the Kenyan authorities rolled out Covid-19 measures, President Kenyatta announced that the government had allocated one billion Kenya shillings ($100 million) toward hiring more skilled health workers.
The next month, the media reported that the government aimed to recruit 6,000 more doctors, nurses, and clinical officers. On May 23, 2020, the president said that the government was going to hire “another 5,000 healthcare workers with diploma and certificate qualifications” making a total of 11,000 newly recruited doctors, nurses, and clinical officers to enhance the government’s “Covid-19 response capability.” Instead of hiring the promised additional 11,000 health workers, the authorities, without explanation, only contracted less than 1,000 nurses and only for one year.
These new recruits were deployed across the nation, so each county only received about 10 additional nurses. Human Rights Watch found that the terms under which the new staff were hired, as well as the delay in the payment of their salaries for up to six months, seriously injured their morale. At the time, Kenya was reporting more than 700 positive cases daily. All doctors and nurses interviewed said that public health facilities remained overstretched and health workers overworked. A senior official of the Kenya National Union of Nurses said that some health workers even left the country: There is a lot of brain drain of health workers, with the majority heading to Canada and the UK.
The resultant shortage exerts a huge strain on the few workers left behind.
The World Health Organization (WHO) patient to nurse ratio is 1 to 6, but in Kenya, the ratio is about 1 to 30.
The strain became even worse in the face of the pandemic. Lack of Health Insurance, Benevolent Fund Human Rights Watch learned that the authorities have not provided affordable health care for health workers who are constantly exposed to the risk of contracting Covid-19.
The health workers interviewed said that authorities ignored their appeals to create – in the absence of universal health coverage – a benevolent fund to offset the bills of nurses and doctors infected with Covid-19 while on duty and to take care of the needs of the families of frontline health workers who die from Covid-19. Kenya has a responsibility to ensure that everyone has access to affordable and reliable health care, not just a few who can afford the current high cost of insurance premiums. The authorities have not honored their pledge to ensure that all health workers have life insurance either, despite the pandemic’s high death rates. By October 3, more than 5,131 people had died of Covid-19 in Kenya. All the interviewed health workers felt concerned that the government, the biggest employer of health workers, failed to provide all its health workers with health and life insurance. A doctor who works as an administrator at the Health Ministry said that the government’s failure to provide health workers with life insurance allowed most private hospitals to do the same. A nurse in Mombasa described the situation: If, as a government employee, I were to get Covid-19 today, I will be taken to a government facility, the same place where I work, and asked to pay from my pocket. I cannot afford it because our salaries are very low. One doctor said of health workers who caught Covid-19 in the course of their work: “We have situations where colleagues were detained in hospitals over Covid-19-related bills and the bodies of our departed colleagues were detained because families could not afford the bills.” The government finally released an undisclosed sum of money to cover Covid-19-related hospitalization and deaths in November 2020; it was a one-off occurrence covering only cases of up to that period, said a senior government doctor and two union officials. Inadequate Remuneration At the outset of the Covid-19 pandemic, the Kenyan authorities promised to introduce Covid-19 risk allowances for all frontline health care workers in the fight against Covid-19, which would be greater than the normal risk allowances introduced in 2016 for health workers, also in response to a strike. Previously, doctors received Ksh5,000 ($50) as a monthly risk allowance while nurses received Ksh3,500 ($35).
The intended Covid-19 risk allowances would have increased the monthly risk allowance for doctors to Ksh20,000 ($200) and for nurses to Ksh15,000 ($150). Doctors, nurses, and clinical officers interviewed said that the authorities first delayed the payment of these allowances for three months, until July 2020, when they only made one-off payments of Ksh20,000 to doctors, Ksh15,000 to nurses, and Ksh10,000 to other health workers working in government hospitals during the pandemic. Since then, the authorities have without explanation failed to pay further Covid-19 risk allowances.
The health workers hired to boost the Covid-19 response were excluded from these payments. All health workers interviewed said that the authorities did not compensate them for prolonged periods at work, including extended work hours and days.
They said that during the first four months of the pandemic, nurses were locked in the isolation wards with patients for two weeks, then went into quarantine for another two weeks before they could rejoin their families.
They said that since July 2020, nurses have remained in the wards for just one week, and then they can return home without quarantining. “It is very unfair to all health workers, but mostly to nurses,” a nurse in Nairobi said about the lack of extra compensation. “Since the outbreak of Covid-19, it is the nurses who have been kept away from their families for long periods without compensation or allowances.” Lack of Psychosocial Support While health workers experienced increasing mental strain, especially as infection numbers continued to rise, they have had no psychosocial support system.
The officials of health associations and unions said that they raised this concern with the relevant authorities numerous times without result. The health workers attributed the mental strain to a combination of factors, most of which they believed were preventable had the government responded better.
The people interviewed said that these causes included overwork, understaffing, inadequate compensation, and the lack of government assistance for those infected with Covid-19 or for the families of health workers who died from Covid-19. An official of the Kenya Medical Practitioners and Dentists Union (KMPDU) noted that many people, including health workers and government officials, suffered from the psychological effects of Covid-19.
The lack of protective facilities caused panic among staff, while the transfer of staff from other wards without any training or counseling as well as the stigmatization of those working in isolation wards exacerbated the mental strain. He said that he was quite shocked to see his colleagues avoiding health workers in the Covid-19 wards for fear of infection. Furthermore, since the government did not provide safe transportation services for health workers, interviewees said they risked being infected on public transportation to get to work when Covid-19 infection rates were peaking. An official of the Kenya Progressive Nurses Association (KPNA) said: “The authorities argued that there was no plan for transport for health workers from the start and could not be factored into the budget that quickly. But there was money specifically allocated for Covid-19, and we expected that this should have been used on transport.” The secretary of the KPNA said that many health workers’ mental health worsened when prices of goods and services, including transportation, increased during the pandemic, and the transportation allowance was no longer enough. In addition, public vehicles were unavailable, following government directive for public vehicles to operate at half capacity, causing most people to report late to work, for which management would admonish them, adding to their stress. One doctor and four nurses said they even experienced mental breakdowns, with nurses saying at least one of their colleagues had attempted suicide. “At some point, we had to try and counsel colleagues, yet we don’t have any experience in counseling,” said a Nairobi-based nurse. “The government wasn’t just willing to provide psychosocial support no matter how much we tried.” Inadequate Countrywide Testing, Information Management Human Rights Watch found that, while they established numerous testing centers across the country, the authorities did not ensure an adequate supply of testing reagents and kits to control the spread of the virus that causes Covid-19. A Nairobi-based laboratory expert working in one of the government’s testing centers and two other doctors said that they lacked guidelines on who should be tested, adding that it was impossible to test everyone because of limited testing kits and reagents. A doctor in Nairobi said: The government started saying we should test only those who show symptoms to cope with limited test kits.
The numbers we are testing are far lower than we should be doing. We are only testing those who show symptoms or those who want to travel. People are now vaccinating without testing to know their status. Yet if you are positive with Covid and get vaccinated, the situation gets aggravated. We have lost people this way, including healthcare workers. Because of undertesting, the laboratory expert questioned the accuracy of the numbers of Covid-19 cases that the Health Ministry reported daily. “Most of the time, reagents have been in short supply,” he said. “Testing patterns [or the size of samples] have been an issue, in some instances giving the notion it’s linked to funding.” The doctors interviewed said that at the beginning of the pandemic, the government set up three laboratories at the National Influenza Center, Kenya Medical Research Institute (KEMRI) in Nairobi the capital; Kilifi, on the east coast; and Kisumu in the southwest. After July 2020, the authorities created more labs in Bungoma, in western Kenya; at the Walter Reed Institute in Kericho, in the Rift Valley region; and at the Coast Provincial Hospital in Mombasa, on the east coast. Later, KEMRI started another lab in Alupe, in the west. Unfortunately, the doctors said that this expansion did not come with measures to ensure the necessary quality of services, including the authorities’ failure to employ enough staff to run the laboratories or to provide supplies to keep them operational. When reagents became unavailable, interviewees said, testing decreased and its quality became compromised. Doctors and managers working at testing facilities said that between March and April 2020, they tested an average of 400 samples per day. In May, June, and early July, the number of tests skyrocketed to 10,000 samples per day. However, by mid-July, the facilities began running out of testing kits and reagents, causing testing to slow down. Between October to December, the centers used up all the reagents, so the government had to cease testing. In January and February 2021, despite the fact that the government had fresh supplies of testing kits by then, the testing remained low because of the doctors’ and nurses’ strike. Testing resumed in March 2021 after the strike had ended. The laboratory expert said that between July and December 2020, when government facilities gradually stopped testing, the authorities reported only the testing results from private hospitals.
The low number of results reported during this period was due to reduced testing and not any decrease in the number of infections.
Read the full article at the original website
References:
- https://www.hrw.org/africa/kenya
- https://www.mfa.go.ke/wp-content/uploads/2020/04/presidential-address-enhanced-measures-in-response-to-the-COVID-19-pandemic-6th-April-2020.pdf
- https://www.sabcnews.com/sabcnews/kenyas-president-orders-investigations-into-alleged-theft-of-covid-19-funds/
- https://www.hrw.org/about/people/otsieno-namwaya
- https://www.health.go.ke/wp-content/uploads/2020/10/October-29-COVID-19-Statement.pdf
- https://www.ohchr.org/en/professionalinterest/pages/cescr.aspx
- https://www.achpr.org/public/Document/file/English/achpr_instr_guide_draft_esc_rights_eng.pdf
- https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:C155
- https://www.imf.org/en/News/Articles/2020/05/06/pr20208-kenya-imf-executive-board-approves-us-million-disbursement-address-impact-covid-19-pandemic
- https://www.worldbank.org/en/news/press-release/2020/04/02/kenya-receives-50-million-world-bank-group-support-to-address-covid-19-pandemic
- http://www.parliament.go.ke/sites/default/files/2021-02/The%20third%20Quarterly%20report%20convering%20the%20period%20from%201st%20july%20to%2030th%20September%202020%20from%20Ethics%20and%20Anti%20-%20Corruption%20Commission.pdf
- https://unmasked.nation.africa/issues/covid19millionaires/kemsa-suspends-ceo-2-directors-over-covid-19-procurements-probe
- https://www.mfa.go.ke/wp-content/uploads/2020/03/presidential-address-25th-march-2020.pdf
- https://www.businessdailyafrica.com/bd/news/covid-19-kenya-begins-hiring-of-6-000-more-health-workers-2285910
- https://www.youtube.com/watch?v=WbHKBt2mytY
- https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/kenya/
- https://allafrica.com/stories/202004170753.html
- https://www.standardmedia.co.ke/counties/article/2001379748/all-set-for-healthcare-workers-covid-19-allowances
